How Medicaid Funding Cuts Force IDD Facilities to Reduce Software Spending
The Intellectual and Developmental Disability (IDD) service sector faces an unprecedented crisis as federal Medicaid cuts threaten the financial viability of facilities nationwide. With 87% of the $80.6 billion spent on IDD services in 2021 coming from Medicaid funding, proposed cuts represent more than a budget adjustment—they create a cascade of operational impacts that directly force facilities to eliminate technology investments and consolidate software systems.
The Scale and Immediacy of Federal Medicaid Cuts
Congressional proposals to slash Medicaid funding by $880 billion over the next decade represent a 16% reduction in federal support, with the Congressional Budget Office projecting that 10.3 million people could lose Medicaid coverage. These cuts, potentially beginning in 2026, would fundamentally reshape how IDD facilities operate, as virtually all 55,000 individuals with disabilities residing in the nation's 5,300 intermediate care facilities are on Medicaid.
The scope of these reductions extends beyond simple percentage cuts. The proposed changes include burdensome work reporting requirements, reduced retroactive coverage from three months to one month, and caps on federal matching rates that would shift costs directly to states. For IDD facilities already operating on razor-thin margins, these changes create immediate pressure to reduce operational expenses wherever possible.
IDD Facilities' Critical Dependence on Medicaid Revenue
IDD facilities operate within a unique financial structure where Medicaid reimbursement often falls short of covering actual care costs, even before any proposed cuts. The average monthly cost per resident ranges from $3,985 for community-based settings to $13,917 for residential habilitation centers, with the vast majority of this funding coming from federal and state Medicaid programs. When Medicaid reimbursement rates decline, facilities face an immediate revenue shortfall that must be addressed through cost reductions.
The financial vulnerability of IDD facilities is already evident in closure statistics. Between January 2023 and February 2024, Texas alone saw 179 Home and Community Services (HCS) homes and 50 Intermediate Care Facility (ICF) facilities permanently close, with another 92 HCS homes and 34 ICF facilities at risk of closure. These closures directly correlate with insufficient Medicaid reimbursement rates, demonstrating how funding pressures translate into operational decisions.
Operational Cost Structure and Reduction Priorities
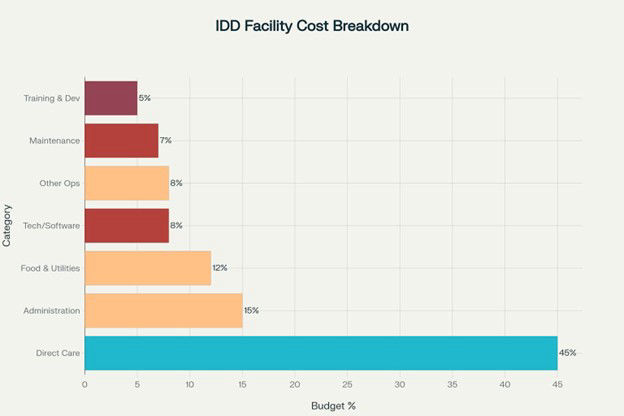
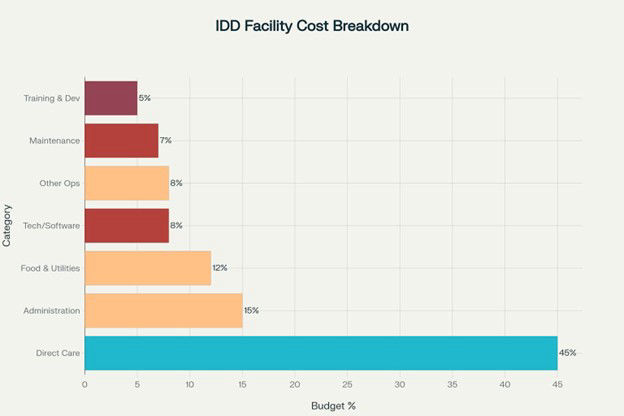
When faced with budget cuts, IDD facilities follow predictable patterns in prioritizing cost reductions based on their operational structure and regulatory requirements. Direct care services, which typically represent 45% of facility budgets, are protected due to state regulations and resident safety requirements. However, administrative functions, technology systems, and support services become immediate targets for reduction.
IDD Facility Cost Breakdown and Cut Priorities During Medicaid Funding Reductions
Healthcare facilities typically spend 3.0-5.9% of their total revenue on information technology, with IDD facilities falling within this range despite their more constrained budgets. During funding crises, technology spending becomes particularly vulnerable because software systems are viewed as operational expenses rather than direct care necessities. Research shows that during healthcare budget cuts, technology investments can be reduced by 50-75% as facilities prioritize immediate operational needs over long-term efficiency gains.
The Software Spending Reduction Process
IDD facilities typically operate with multiple software systems serving different functions: Electronic Health Records (EHR), medication management (eMAR), billing and claims processing, staff scheduling, compliance tracking, communication platforms, maintenance management, and financial oversight. Each system requires separate licensing fees, training costs, and technical support, creating a fragmented technology environment that becomes expensive to maintain during budget constraints.
When Medicaid cuts force operational reductions, software spending follows a predictable elimination pattern. Training and development programs, representing about 5% of facility budgets, are typically eliminated first as they're viewed as non-essential during crisis periods 34. Technology and software systems, comprising approximately 8% of operational costs, become the second priority for cuts because they can be consolidated or eliminated without immediate impact on daily care delivery.
The consolidation process typically involves eliminating specialized software tools and moving to manual processes or basic spreadsheet systems. Facilities often cancel subscriptions to compliance tracking software, automated scheduling systems, and communication platforms, reverting to paper-based documentation and manual processes. This reduction strategy provides immediate cost savings but creates long-term operational inefficiencies and increased compliance risks.
Impact on Operational Efficiency and Compliance
The reduction in software spending creates a cascade of operational problems that ultimately increase facility costs and reduce care quality. Manual documentation processes consume 50% more staff time than electronic systems, forcing facilities to reallocate direct care staff to administrative tasks. This reallocation reduces the time available for resident care and increases the risk of burnout among remaining staff members.
Compliance tracking becomes particularly challenging when facilities eliminate automated monitoring systems. IDD facilities must maintain detailed records for state certification, Medicaid billing, and resident safety protocols. Without software systems to manage these requirements, facilities face increased risk of regulatory violations, which can result in additional financial penalties and potential closure.
The elimination of integrated billing and claims processing software creates additional financial pressures. Manual billing processes increase claim rework costs by 42% and delay reimbursement cycles, further straining facility cash flow during already difficult financial periods. These delays compound the original Medicaid funding problems, creating a downward spiral of financial instability.
Long-term Consequences for Facility Viability
The forced reduction in software spending represents more than a temporary cost-cutting measure—it fundamentally undermines facility operational capacity and competitive positioning. Facilities operating with outdated or eliminated technology systems cannot compete effectively for staff, residents, or contracts with organizations that maintain modern operational infrastructure.
The inability to invest in technology also prevents facilities from adapting to changing regulatory requirements and industry standards. As the healthcare sector increasingly emphasizes electronic documentation, telehealth capabilities, and data-driven care planning, facilities without adequate software systems become increasingly isolated from best practices and innovation.
Most critically, the reduction in software spending during Medicaid cuts creates a permanent disadvantage that persists even if funding is restored. Facilities that eliminate technology infrastructure during crisis periods often lack the capital and expertise to rebuild these systems when financial conditions improve, leaving them permanently disadvantaged in an increasingly technology-dependent healthcare environment.
The Strategic Imperative for Technology Consolidation
Rather than eliminating technology systems entirely, forward-thinking IDD facilities are recognizing that consolidating multiple software functions into comprehensive platforms represents the most effective response to Medicaid funding pressures. This approach maintains operational efficiency while achieving the cost reductions necessary to survive funding cuts.
The transition from multiple point solutions to integrated platforms can reduce software licensing costs by $50,000-$150,000 annually for large facilities while maintaining all essential operational functions 17. For smaller facilities, consolidation can eliminate $2,000-$5,000 in monthly software expenses while actually improving operational efficiency through integrated workflows.
Furthermore, facilities maintaining siloed systems will face unavoidable service reductions, while those adopting unified platforms achieve:
• 18-24% lower operational costs through automated prior authorization and claims processing
• 9-14% occupancy rate improvements from streamlined family communication tools
The financial urgency is clear: Every month of delayed integration costs mid-sized facilities $7,200-$15,000 in preventable expenses – equivalent to 2-4 resident service days lost monthly.
This strategic approach to software spending allows facilities to maintain compliance capabilities, preserve staff efficiency, and position themselves for growth when funding stabilizes, rather than simply eliminating technology investments and accepting permanent operational disadvantages.
Conclusion
Medicaid funding cuts create an inevitable cascade effect that forces IDD facilities to reduce software spending as part of broader operational cost reductions. With 87% of IDD funding dependent on Medicaid and proposed cuts of $880 billion over the next decade, facilities face immediate pressure to eliminate what they perceive as non-essential technology expenses. However, the most successful facilities will recognize that strategic technology consolidation, rather than elimination, provides the path to maintaining operational efficiency while achieving necessary cost reductions during this challenging funding environment.